Ethosuximide (Zarontin): Uses, Dosage, Side Effects, Interactions & Monitoring for Absence Seizures
GET HELP TODAY!
100% Confidentiality Guaranteed

Drug Information
Brand / names: Zarontin, Ethosuccimide, Ethylmethylsuccimide, Emeside, Petinimid
Drug class: Anticonvulsants and Antiseizure
About the Author
Mat Gorman
Mat Gorman is an experienced mental health writer and medical researcher with over a decade of experience in addiction recovery education. He specializes in translating complex clinical topics into clear, compassionate content that empowers families and individuals seeking treatment. Mat has collaborated with recovery centers, licensed therapists, and physicians to publish evidence-based resources across the behavioral health space. His passion for helping others began after witnessing the struggles of loved ones facing substance use disorder. He now uses his platform to promote hope, clarity, and long-term healing through accurate, stigma-free information.
Ethosuximide Overview at a Glance
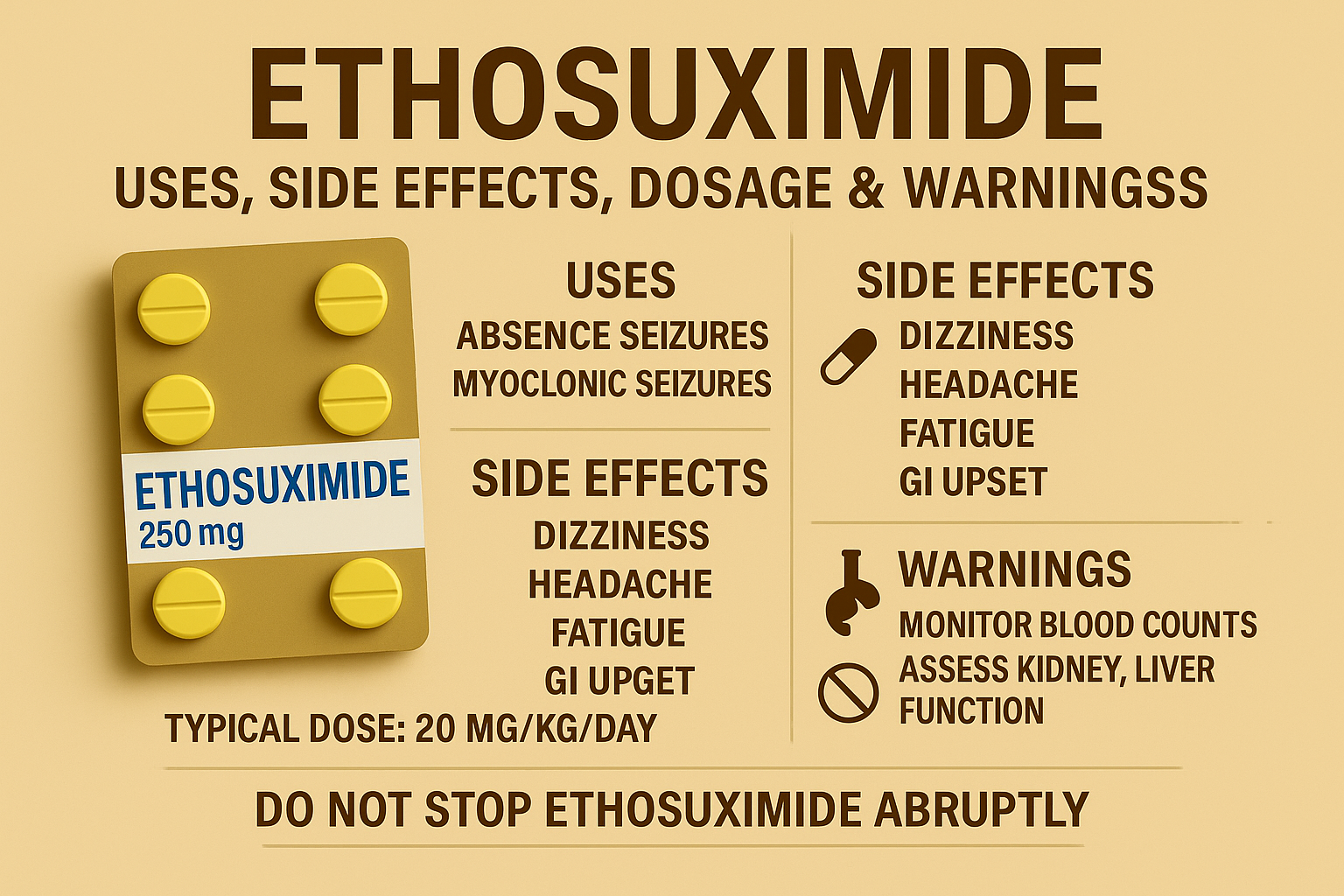
- What it is: Ethosuximide is a succinimide anti‑seizure medication used primarily for absence (petit mal) seizures. Brand: Zarontin.
- Role in therapy: Considered first‑line for childhood absence epilepsy; in a major randomized trial, ethosuximide and valproate were more effective than lamotrigine, with fewer attentional side effects on ethosuximide.
- How it works: Reduces abnormal thalamic firing by blocking T‑type calcium channels.
- Typical adult start: 500 mg once daily, titrating by 250 mg every 4–7 days; max ~1,500 mg/day (often divided). Therapeutic range: 40–100 μg/mL. Steady state: ~4–7 days.
- Common side effects: GI upset (nausea, vomiting, abdominal pain), drowsiness/dizziness, headache, hiccups—often improving after the first couple of weeks.
- Serious warnings: Rare blood dyscrasias, serious skin reactions (SJS/DRESS), lupus‑like syndrome, and suicidality; do not stop abruptly.
What Is Ethosuximide?
Ethosuximide is an FDA‑approved anti‑seizure medicine that controls absence seizures, characterized by brief lapses in awareness or “staring spells.” It is available as 250 mg capsules and 250 mg/5 mL oral solution. In practice, it is most often used in children and adolescents with absence epilepsy, and it can be useful in adults with the same seizure type.
How Ethosuximide Works
Absence seizures arise from pathological oscillations in thalamo‑cortical networks. Ethosuximide dampens these oscillations primarily by blocking low‑threshold T‑type calcium channels in thalamic neurons. That reduces the 3‑Hz spike‑and‑wave discharges typical of absence seizures, helping prevent the brief periods of impaired awareness.










Indications & Role in Therapy
- Primary indication: Control of absence (petit mal) seizures. It is not broadly effective for other generalized seizures (e.g., tonic‑clonic) and may even worsen them in some mixed‑syndrome cases, so clinicians confirm seizure type before initiating therapy.
- First‑line status: In a landmark NEJM randomized trial of children with new‑onset absence epilepsy, ethosuximide and valproic acid were more effective than lamotrigine for seizure control after 16 weeks; ethosuximide produced fewer attentional side effects than valproic acid, supporting its first‑line use when absence seizures occur without generalized tonic‑clonic seizures.
Dosing & Administration
Do not start, stop, or change doses without medical supervision. Abrupt discontinuation can precipitate seizures and, rarely, status epilepticus.
Adult Dosing (absence seizures)
- Initial: 500 mg once daily
Titration: Increase by 250 mg every 4–7 days as needed/tolerated - Maintenance: Individualized to effect; often 1,000–1,500 mg/day in 1–2 divided doses
- Maximum: ~1,500 mg/day (some sources note higher carefully supervised doses)
- Therapeutic range: 40–100 μg/mL serum; steady state typically in 4–7 days after a dose change.
Pediatric Dosing
- Age <3 years: Safety/efficacy not established.
- Ages 3–6 years: 250 mg once daily to start; titrate by 250 mg every 4–7 days to effect
- ≥6 years: Often same as adults (start 500 mg once daily, titrate by 250 mg every 4–7 days)
- Weight‑based guidance: Many children respond around ~20 mg/kg/day; some require higher (up to ~40 mg/kg/day) to reach therapeutic levels under close supervision.
Administration Tips
- May be taken with food to reduce GI upset.
- Oral solution: measure doses precisely using a calibrated device.
- Divided dosing can improve tolerability at higher totals.
Missed Dose / Tapering
- Missed dose: Take when remembered unless near the next dose—then skip; do not double up.
- Tapering: When discontinuation is appropriate, reduce gradually under clinician guidance.
Side Effects
Common (often early and dose‑related)
- Gastrointestinal: nausea, vomiting, abdominal pain/cramps, loss of appetite
- Neurologic/CNS: drowsiness, dizziness, headache; hiccups have been reported
These frequently improve as the body adjusts over 1–2 weeks; taking with food and slow titration can help.
Serious (seek urgent care)
- Severe skin reactions: Stevens‑Johnson syndrome (SJS) and DRESS—stop the drug and get immediate medical care if rash, blistering, mucosal sores, fever, or facial swelling occur.
- Blood dyscrasias: rare but potentially life‑threatening (e.g., leukopenia, agranulocytosis, aplastic anemia); report sore throat, fever, easy bruising/bleeding promptly.
- Systemic lupus erythematosus (SLE)–like reactions: report chest pain, joint pain, fever, rash, hair loss, or breathing trouble.
- Psychiatric effects: monitor for new or worsening depression, suicidal thoughts, agitation, or abnormal behaviors; contact a clinician if these emerge.
- Worsening/appearance of generalized tonic‑clonic seizures in mixed epilepsies has been reported; clinicians choose therapy based on seizure types.
Warnings & Precautions
- Do not stop suddenly. Slow dose changes under supervision are standard to avoid rebound seizures.
- Hematologic, hepatic, renal monitoring is advisable (see Monitoring). Use extreme caution in existing liver/renal disease.
- Driving/Operating machinery: dizziness or somnolence can impair performance—assess individual response first.
Drug Interactions (selected, not exhaustive)
- Valproic acid may increase or decrease ethosuximide levels (monitor, adjust if needed).
- Ethosuximide may elevate phenytoin concentrations (check levels if combined).
- CNS depressants (e.g., meclizine, phenobarbital, sedating antihistamines, alcohol, cannabis) can increase sedation; monitor closely.
- Ginkgo and other supplements may interact—disclose all OTC/herbals to your clinician.
More Time. More Joy. More You. Start Now.
WE ACCEPT MOST INSURANCES




Monitoring & Therapeutic Drug Monitoring (TDM)
- Baseline and periodic labs: CBC, liver function tests, and urinalysis are commonly recommended due to rare but serious hematologic, hepatic, and renal adverse effects.
- Serum ethosuximide levels: Target 40–100 μg/mL (may individualize). Levels assist when seizures persist, side effects occur, adherence is uncertain, or interacting drugs are added.
Special Populations
Pregnancy
Ethosuximide crosses the placenta. As with many anti‑seizure medicines (ASMs), there are reports of increased risk of birth defects with in‑utero ASM exposure; absolute risks and comparative safety profiles differ across agents. Decisions balance seizure control (critical in pregnancy) against potential risks, and often involve specialists. If pregnancy is planned or occurs, consultation and possible enrollment in a pregnancy registry are advised.
Breastfeeding
Ethosuximide appears in breast milk—infant serum levels can be a substantial fraction of maternal levels in some reports. While adverse events are uncommon, clinicians may advise monitoring infants for sedation, feeding difficulty, and weight gain issues. Overall, many expert groups encourage breastfeeding with appropriate monitoring due to its benefits.
Hepatic or Renal Impairment
Use caution and monitor more closely; dose adjustments may be needed.
Pediatrics
Safety is not established below age 3 years; otherwise, ethosuximide is widely used in children with absence epilepsy and is a first‑line choice when absence seizures occur without generalized tonic‑clonic seizures.
Pharmacology & Kinetics
- Mechanism: Inhibits T‑type calcium channels within thalamic relay neurons, stabilizing thalamo‑cortical network excitability.
- Half‑life: Approximately 50–60 hours in adults and ~30 hours in children; inter‑individual variability exists.
- Steady state: Typically 4–7 days after a dosing change (long half‑life).
Freedom Starts Here. Take Back Your Life Today.
Same-Day Admissions in Austin Available.
Comparisons & Alternatives
- Ethosuximide vs Valproate: Comparable short‑term efficacy for absence seizures; ethosuximide tends to have fewer attentional adverse effects than valproate, which may influence first‑line selection in pure absence epilepsy. Valproate may be preferred if other generalized seizure types coexist.
- Ethosuximide vs Lamotrigine: Ethosuximide generally outperforms lamotrigine for initial control of typical absence seizures in randomized data.
Practical Tips for Patients & Caregivers
- Adherence matters: Take it at the same time daily; titrate slowly if advised.
- Report concerning symptoms early: fever, sore throat, rash, bruising/bleeding, mood changes.
- No abrupt stop: If therapy must change, your clinician will create a taper.
- Storage: Keep at room temperature away from moisture/heat; protect oral solution from freezing/light.
Frequently Asked Questions About Ethosuximide and Addiction
What are the side effects of Ethosuximide?
Common side effects include nausea, drowsiness, dizziness, and fatigue. More serious risks include blood disorders, severe skin reactions, and suicidal thoughts, which require immediate medical attention.
What is the mechanism of action of Ethosuximide?
Ethosuximide works by blocking T-type calcium channels in the thalamus, reducing abnormal brain activity that causes absence seizures.
Is Ethosuximide safe for children?
Yes, Ethosuximide is considered a first-line treatment for childhood absence epilepsy, but it should always be prescribed and monitored by a pediatric neurologist.
What is the black box warning for Ethosuximide?
Ethosuximide carries a warning about the risk of suicidal behavior and ideation, requiring careful monitoring of mood and behavior changes.
What defines an addiction?
Addiction is characterized by compulsive drug use despite harmful consequences, often involving physical dependence and psychological cravings.
What are 5 signs of an addiction?
Warning signs include loss of control, cravings, neglect of responsibilities, withdrawal symptoms, and continued use despite harm.
How to get rid of addiction?
Treatment may involve medical detox, behavioral therapy, counseling, support groups, and long-term relapse prevention strategies.
What are the 4 elements of addiction?
The core elements are cravings, loss of control, tolerance, and withdrawal, which together sustain the cycle of addiction.
Can Ethosuximide be addictive?
While Ethosuximide is not typically associated with euphoria, misuse or abrupt discontinuation can lead to dependence and withdrawal symptoms, requiring medical supervision.
How can Nova Recovery Center help with Ethosuximide abuse?
Nova Recovery Center provides medically supervised detox, individualized treatment plans, and long-term recovery programs to address Ethosuximide misuse and build a foundation for lasting sobriety.
How Nova Recovery Center Helps with Ethosuximide Addiction and Abuse
Nova Recovery Center provides compassionate, evidence-based care for individuals struggling with Ethosuximide addiction and abuse. While Ethosuximide is most often prescribed to treat absence seizures, misuse of this medication can lead to dependence, withdrawal challenges, and serious health risks. At Nova, clients begin with a safe, medically supervised detox to manage symptoms and stabilize the body. From there, our treatment team develops personalized plans that address not only physical dependence but also the emotional and behavioral patterns tied to substance use. We offer a full continuum of care that includes residential treatment, intensive outpatient programs, and sober living support. Clients also engage in evidence-based therapies, relapse prevention training, and holistic practices to strengthen long-term recovery. Our programs emphasize accountability, structure, and peer support—key elements for lasting change. With licensed clinicians, recovery specialists, and a supportive community, Nova Recovery Center helps individuals rebuild healthier lives free from medication misuse. Ultimately, our goal is to guide clients toward long-term sobriety, improved well-being, and renewed hope for the future.
Get help today. Reach out now to start your path to healing.
- Glauser, Tracy A., et al. “Ethosuximide, Valproic Acid, and Lamotrigine in Childhood Absence Epilepsy.” The New England Journal of Medicine, 4 Mar. 2010. https://www.nejm.org/doi/full/10.1056/NEJMoa0902014
- “Ethosuximide (Oral Route).” Mayo Clinic, updated 1 Aug. 2025. https://www.mayoclinic.org/drugs-supplements/ethosuximide-oral-route/description/drg-20072587
- “Ethosuximide Dosage Guide + Max Dose, Adjustments.” Drugs.com, updated 15 July 2025. https://www.drugs.com/dosage/ethosuximide.html
- “ZARONTIN (Ethosuximide) Prescribing Information.” U.S. Food and Drug Administration (accessdata.fda.gov), 2016. https://www.accessdata.fda.gov/drugsatfda_docs/label/2016/012380s036lbl.pdf
- “ZARONTIN—Ethosuximide Capsule: Medication Guide and Label.” DailyMed, U.S. National Library of Medicine. https://dailymed.nlm.nih.gov/dailymed/medguide.cfm?setid=0e008f33-70a1-4bc6-b3a0-d45214418ab6 and related label entries.
- Hanrahan, B. “Ethosuximide.” StatPearls, NCBI Bookshelf, updated 2024. https://www.ncbi.nlm.nih.gov/books/NBK544244/
- “Ethosuximide.” MedlinePlus Drug Information. https://medlineplus.gov/druginfo/meds/a682327.html
- “Ethosuximide (Zarontin) – Epilepsy Medication.” Epilepsy Foundation (epilepsy.com), 16 Oct. 2023. https://www.epilepsy.com/tools-resources/seizure-medication-list/ethosuximide
- “Ethosuximide.” WebMD, 21 Feb. 2025. https://www.webmd.com/drugs/2/drug-7098/zarontin-oral/details
- “Ethosuximide – Drugs and Lactation Database (LactMed).” NCBI Bookshelf, updated 15 Aug. 2024. https://www.ncbi.nlm.nih.gov/books/NBK501219/
Other Outpatient Drug and Alcohol Rehab Locations
Medical Disclaimer
The information on this page is provided for educational purposes only and should not be used as a substitute for professional medical advice, diagnosis, or treatment. Ethosuximide and other prescription medications must only be taken under the guidance of a licensed healthcare provider. Do not begin, stop, or adjust your dosage without consulting your doctor. If you experience severe side effects, withdrawal symptoms, or thoughts of self-harm, call 911 immediately in the United States or seek emergency medical care. For mental health support, you can also dial 988 to connect with the Suicide & Crisis Lifeline, available 24/7.
Nova Recovery Center Editorial Guidelines
By instituting a policy, we create a standardized approach to how we create, verify, and distribute all content and resources we produce. An editorial policy helps us ensure that any material our writing and clinical team create, both online and in print, meets or exceeds our standards of integrity and accuracy. Our goal is to demonstrate our commitment to education and patient support by creating valuable resources within our realm of expertise, verifying them for accuracy, and providing relevant, respectful, and insightful data to our clients and families.

