What “pregnancy category X” means
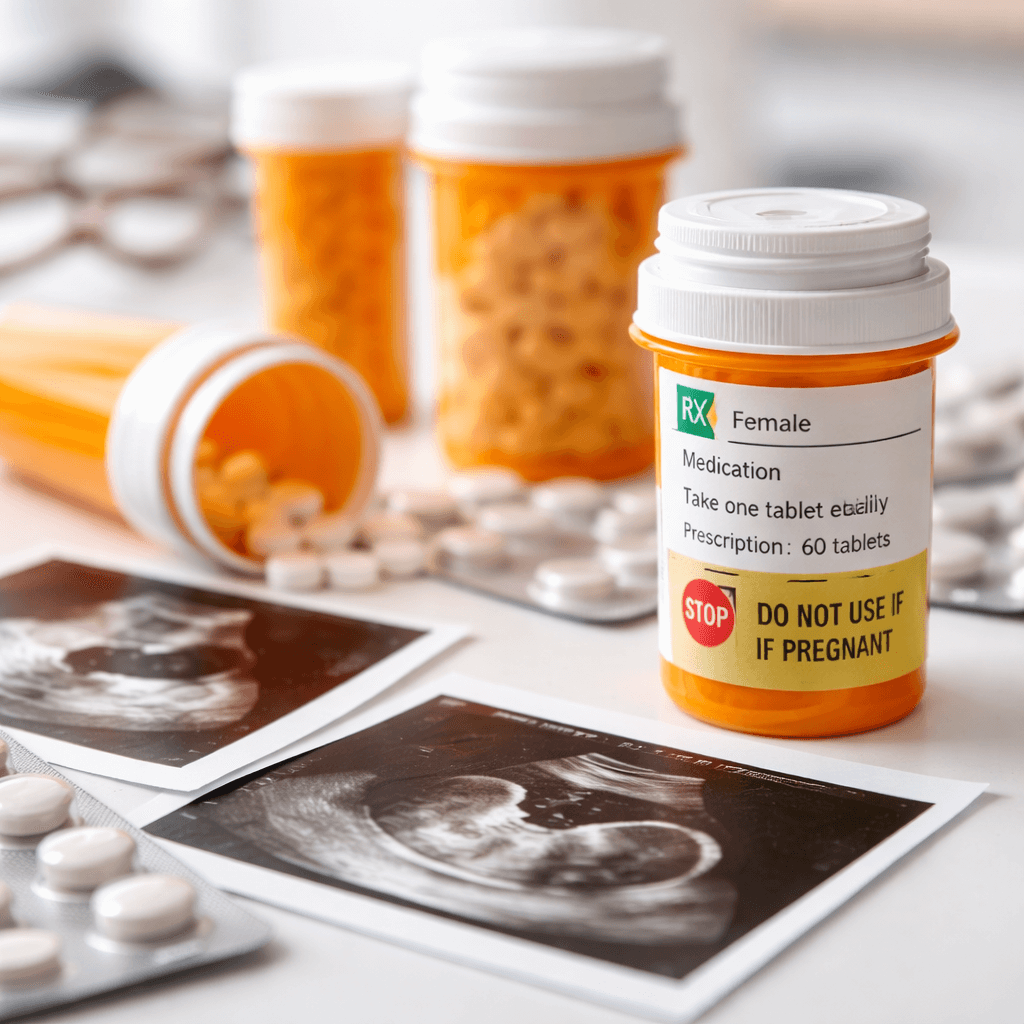
In the letter system, pregnancy category X meant a drug is contraindicated in pregnancy, or in plain terms, it was a “do not use if pregnant” label. The definition focused on two points: there is evidence of fetal harm, and the risk clearly outweighs any possible benefit for a pregnant person.
If you want the official wording used in the old system, the federal reference at HHS pregnancy category definitions explains what Category X meant.
Category X also signaled prevention, since many drugs in this group require pregnancy testing, reliable birth control, or both because early exposure can matter. If you are of childbearing age and take one of these medicines, your doctor may talk with you about planning, timing, and safer options.
Pregnancy medication categories: C, D, and X
People also search for pregnancy class C, pregnancy category D (or pregnancy class D), and Category X when comparing risks, so here is a simple way to read the older letters.
- Pregnancy class C: Risk is possible, but not clear. Animal studies may show harm, and there may be limited human data. A doctor may still use it when benefits are judged to be greater than risks.
- Pregnancy category D: There is evidence of human fetal risk. Even so, it may be used for a serious condition when there is no safer choice and the benefit is strong.
- Pregnancy category X: The risk is clear and the benefit does not justify use in pregnancy. It is generally a “no” for pregnant patients.
Two practical notes help prevent mistakes. First, risk can change by trimester and by dose. Second, the “right” choice is not only about fetal risk, because it also depends on what happens if the parent’s illness is not treated, which is one reason the FDA moved away from letter grades.
For a high-level look at how pregnancy medications categories are discussed in clinical education, the NIH overview on pregnancy medications summarizes the older categories and the newer approach.
If your concern involves substance exposure during pregnancy, not just prescribed medications, you may also want to read our guide on newborn withdrawal symptoms (NAS).
Why there isn’t one perfect pregnancy category X drugs list
It is tempting to look for one official list that answers everything, but a static “pregnancy category X drugs list” has limits for three reasons.
- The FDA replaced the letter system, so many newer labels do not show C, D, or X at all.
- Labels evolve, which means pregnancy warnings and guidance can change as new data appears.
- Risk depends on context, because the same drug may carry different risk based on dose, route, and when in pregnancy exposure happens.
The most reliable step is to use the current drug label and a clinician’s risk–benefit review. The FDA explains the newer labeling approach on its Pregnancy and Lactation Labeling Resources page.
How to check your medication’s pregnancy warning today
If you are trying to get an accurate answer fast, these steps usually help more than a list.
- Bring the exact medication name, dose, and form (tablet, capsule, injection, topical) to your appointment.
- Ask your pharmacist to check the most current label and highlight the pregnancy risk summary.
- Ask your doctor what the risk is for you, based on timing, dose, and your health condition.
- Review all over-the-counter products, vitamins, and herbal supplements too, because “natural” does not always mean safe.
Pregnancy category X drugs list: common examples
Even though the letter system is older, some drugs are often listed as Category X in older references, but the examples below are for education only. Always confirm the current pregnancy warning with your prescriber or pharmacist.
- Oral retinoids used for severe acne (example: isotretinoin): linked with major birth defects, so strict pregnancy prevention rules are common.
- Some immune and cancer drugs (examples: thalidomide and lenalidomide): known for severe fetal harm risk, and pregnancy is usually not allowed during use.
- Methotrexate: used for some autoimmune diseases and other conditions; it can cause serious harm in pregnancy.
- Ribavirin: an antiviral linked with fetal risk; pregnancy avoidance is often advised during treatment and for a period after.
- Finasteride and dutasteride: medicines that can affect fetal development and are generally avoided in pregnancy.
This list is not complete, and it is not a substitute for a personal plan. If you are seeing “X” on a list, treat it as a warning sign to talk with your doctor right away.
What to do if you might be pregnant and you’re taking a Category X medication
If you might be pregnant and you are taking a medicine that was labeled pregnancy category X, act quickly but avoid panic decisions or sudden changes on your own.
- Do not stop on your own. Some medicines need a safe taper, and stopping suddenly can be harmful.
- Call your prescriber and your prenatal provider. Ask what to do today, not “at your next visit.”
- Confirm pregnancy status. Use a home test or in-office test and share the result.
- Ask about next steps. This includes safer options, needed monitoring, and what symptoms should prompt urgent care.
If alcohol, opioids, or sedatives are part of the picture, do not try to quit “cold turkey,” because withdrawal can be medically serious. Medically supervised care can help protect both parent and baby, so learn more about Austin detox if you need help with safe stabilization.
When to get urgent help
If you have severe symptoms, seizures, heavy bleeding, severe abdominal pain, or thoughts of self-harm, seek emergency care right away. If you are not sure what is urgent, call your local emergency number or contact your on-call provider for guidance.
What to ask your doctor about “X” (and “D” and “C”) medications
Bring your questions in writing so you can stay focused when you are stressed or short on time. Consider asking:
- What does the current label say about pregnancy risk? Ask for the risk summary and the key facts behind it.
- Is the risk tied to a specific trimester, dose, or form? Timing and dose can change risk.
- What are safer alternatives? This may include a different medicine, a lower dose, or a non-drug option.
- What is the risk if I do not treat the condition? Untreated illness can also harm pregnancy.
- Do I need birth control or pregnancy tests? This is common with known teratogens.
- How should I switch or taper? Ask for a clear plan and follow-up dates.
- How does this affect breastfeeding? Pregnancy and lactation risks can differ.
If you are managing anxiety, insomnia, depression, or substance use at the same time, tell your doctor. These details can change the safest plan, and you deserve care that supports your pregnancy and your recovery.
Support when substance use is involved
Some people discover pregnancy while also dealing with alcohol or drug use, and in that situation medication decisions can feel even more urgent. It helps to focus on two goals: protect the pregnancy and avoid unsafe withdrawal or relapse.
After stabilization, longer-term treatment can provide therapy, structure, and relapse prevention tools. Learn more about Austin residential inpatient rehab if you are exploring next steps.
Next steps and ongoing support
If you are looking for a setting outside the city, you can explore Wimberley inpatient rehab and ask how pregnancy-related care is coordinated with outside medical providers.
No matter what you take, bring a full list of prescriptions, over-the-counter products, and supplements to every visit, since that single step helps your care team spot hidden risks and choose safer options faster.