Last Updated on January 22, 2026
What “long-term brain effects” means in real life
People use the phrase “brain effects” in different ways. Most concerns fit into three buckets.
- Changes in brain chemicals and their receptors while the medicine is in your system.
- Changes in how the brain adapts to a steady dose over time.
- Changes you can feel, like sleep, focus, motivation, or emotional range.
“Long term” also varies by source. In many studies it means six months or more. In everyday care, long term antidepressant use may last for years.
Plain-language terms you may hear
- Brain chemicals: messengers like serotonin, norepinephrine, and dopamine.
- Receptors: tiny “switches” that sense those messengers and change cell activity.
- Brain adjustment: the brain’s way of restoring balance after a long change.
- Plasticity: the brain’s ability to change with stress, learning, and treatment.
One key caution: depression, anxiety, trauma, poor sleep, and substance use can also change brain function. That makes it hard to pin every change on the medication alone.
What’s known: how antidepressants affect the brain over time
Antidepressants act on brain systems tied to mood and stress. They often take a few weeks to help, which suggests that slower brain adjustment matters.
For a clear overview of antidepressants as part of depression treatment, the National Institute of Mental Health explains typical use and expected timelines: Depression and treatment options (NIMH).
SSRI long term use and serotonin pathways
SSRIs raise serotonin activity between nerve cells. With ssri long term use, the brain can respond by changing receptor sensitivity and related pathways. This kind of adjustment is common in biology and does not, by itself, mean harm.
Serotonin also supports sleep, appetite, sexual function, and how the body handles stress. That is one reason some long-term effects feel mental, even when the whole body is involved.
Different antidepressants can shift different “control knobs”
Some antidepressants affect both serotonin and norepinephrine. Others affect norepinephrine and dopamine. Because these systems link to focus, energy, and reward, people can have different long-term experiences with different meds.
Brain circuits can change, not just chemicals
In brain studies, effective treatment is often linked with shifts in circuits tied to threat response, emotion control, and reward learning. Many studies also find a reduced “negative bias,” meaning the brain reacts less strongly to negative cues. These patterns support the idea that treatment can change how the brain processes information.
How researchers study brain effects and why results can differ
It helps to know what “evidence” means in this area. Researchers use a few main tools, and each has limits.
In general, there are two study types. Randomized trials can test cause and effect, but they are often short. Observational studies can follow people longer, but they cannot fully control for who starts the medication and why.
This is why you may see mixed headlines online. A study might find an “association” between long-term use and a brain measure, but that does not prove the medication caused the change. It may reflect the severity of depression, chronic stress, or other health factors.
Brain scans show patterns, not a personal diagnosis
MRI can measure brain structure, like the size of certain regions. Functional MRI can measure changes in brain activity while a person rests or completes a task. These tools can show group trends, but they cannot prove what one person’s brain “should” look like.
Cognitive tests and symptom scales matter
Many studies also use memory tests, attention tasks, and mood scales. These results are often closer to real life than a scan alone. Still, they can be shaped by sleep, stress, pain, and other medications.
Why it is hard to isolate medication effects
- People who take antidepressants long-term may have more severe symptoms to start.
- Many studies are short, even when the drug is used for years.
- Life events, therapy, and routine changes can shift brain function too.
- Alcohol and drug use can affect the same circuits tied to mood and reward.
Because of these factors, two studies can look at similar people and reach different results. That is why “what’s known” tends to be about broad patterns, not absolute rules.
What’s unclear: permanent change, “brain damage,” and lasting symptoms
People often ask if antidepressants change the brain permanently. Research does not support one simple answer for every person.
It also helps to separate “functional” changes from “structural” injury. Functional changes are shifts in sleep, emotion, or focus. Structural injury is damage from events like stroke, severe head trauma, or oxygen loss. Most concerns linked to antidepressants are about function and quality of life, not clear evidence of injury.
Some studies link successful treatment with changes in brain structure or activity, especially in stress-sensitive areas. But results vary, and it is hard to separate medication effects from illness effects. This PubMed Central review describes the evidence and key limits in this area: Antidepressants and brain structure (PubMed Central).
Reversible, persistent, and permanent are not the same
When people worry about “permanent change,” they may mean different things.
- Reversible: a change that fades after the dose is lowered or the drug is stopped.
- Persistent: a change that lasts longer than expected and improves slowly.
- Permanent: a change that never improves, even with time and support.
Most research is better at finding reversible changes than permanent ones. Long follow-up studies are limited, and people’s lives change a lot over time.
A note on common SSRI questions
A common question is “does Lexapro change your brain permanently.” Lexapro (escitalopram) is an SSRI, so it changes serotonin activity while you take it and the brain adapts. Most evidence does not suggest permanent brain damage in most people, but some people report a longer “settling” phase after stopping. If you are worried, a slow, guided plan with your prescriber is safer than stopping suddenly.
Long term antidepressant side effects that can feel like brain changes
Many long term antidepressant side effects are physical, like nausea or sweating. Others feel like brain changes because they affect emotion, drive, or thinking speed.
A simple way to track “brain side effects”
If you are unsure whether a symptom is from the medication, tracking can help. Write down sleep hours, energy, mood, and focus each day for two weeks. Note any dose changes, missed doses, alcohol or drug use, and major stressors. This record makes it easier for a clinician to spot patterns and adjust care.
Emotional blunting
Some people feel less sadness and less anxiety, but also less joy or connection. This is often called emotional blunting. It may relate to changes in how the brain handles emotion and reward, and it can be dose-related.
Lower motivation or “flat” reward
People may describe lower drive or less excitement about things they usually enjoy. This can be a medication effect, a depression symptom, or both. Tracking when it began and what makes it better can guide the next step.
Brain fog, focus, and memory
Brain fog can include slower thinking, reduced focus, or forgetfulness. These symptoms also show up with depression, anxiety, and poor sleep, so timing matters. If brain fog started after a dose change, the medication may be a factor.
Sleep changes that ripple into the day
Some antidepressants are more activating and can worsen insomnia. Others are more sedating and can cause grogginess. Since sleep drives attention and mood, sleep is a key part of any long-term brain check-in.
If alcohol or other drugs are also in the picture, sleep and mood can swing more sharply. If you need safe medical support for substance withdrawal, Austin detox offers 24/7 monitoring and stabilization.
What’s known about stopping after long term antidepressant use
Long term antidepressant use can lead the brain to expect a steady level of medication. When the dose drops quickly, the brain may react as it rebalances.
If you have taken an antidepressant for a long time, it may be normal for the taper to take longer than you expect. A slower pace can lower the chance that symptoms disrupt work, sleep, or recovery routines. The goal is not speed. The goal is stability.
Many clinicians call this “discontinuation syndrome,” but it is best understood as withdrawal from a drug the brain adapted to. An NIH NCBI Bookshelf clinical update describes antidepressant withdrawal and supports gradual, individualized tapering: Antidepressant withdrawal syndrome (NCBI Bookshelf).
Why withdrawal can look like relapse
Withdrawal and relapse can share symptoms, like anxiety, low mood, sleep trouble, and poor focus. Timing can help: withdrawal often starts soon after a dose drop, while relapse often builds more slowly. A prescriber can help sort this out, especially if symptoms are intense.
Safer taper principles
- A plan made with a prescriber, especially after years of use.
- Slower dose reductions if symptoms show up.
- Stable sleep, meals, and daily routine during the taper.
- Therapy support to manage stress while the brain adjusts.
If you ever feel unsafe, seek urgent help right away. Do not make medication changes alone during a crisis.
When extra support is helpful for brain health and recovery
Sometimes the most important “brain effect” is not the medication alone. It is the mix of depression, anxiety, stress, and substance use all pulling on the same brain systems.
Signs you may need a higher level of care
- You use alcohol or drugs to cope with mood or medication side effects.
- You have strong withdrawal risk from substances.
- Mood symptoms are severe, or daily life feels unsafe or unmanageable.
- You need dual-focus care for substance use and mental health symptoms.
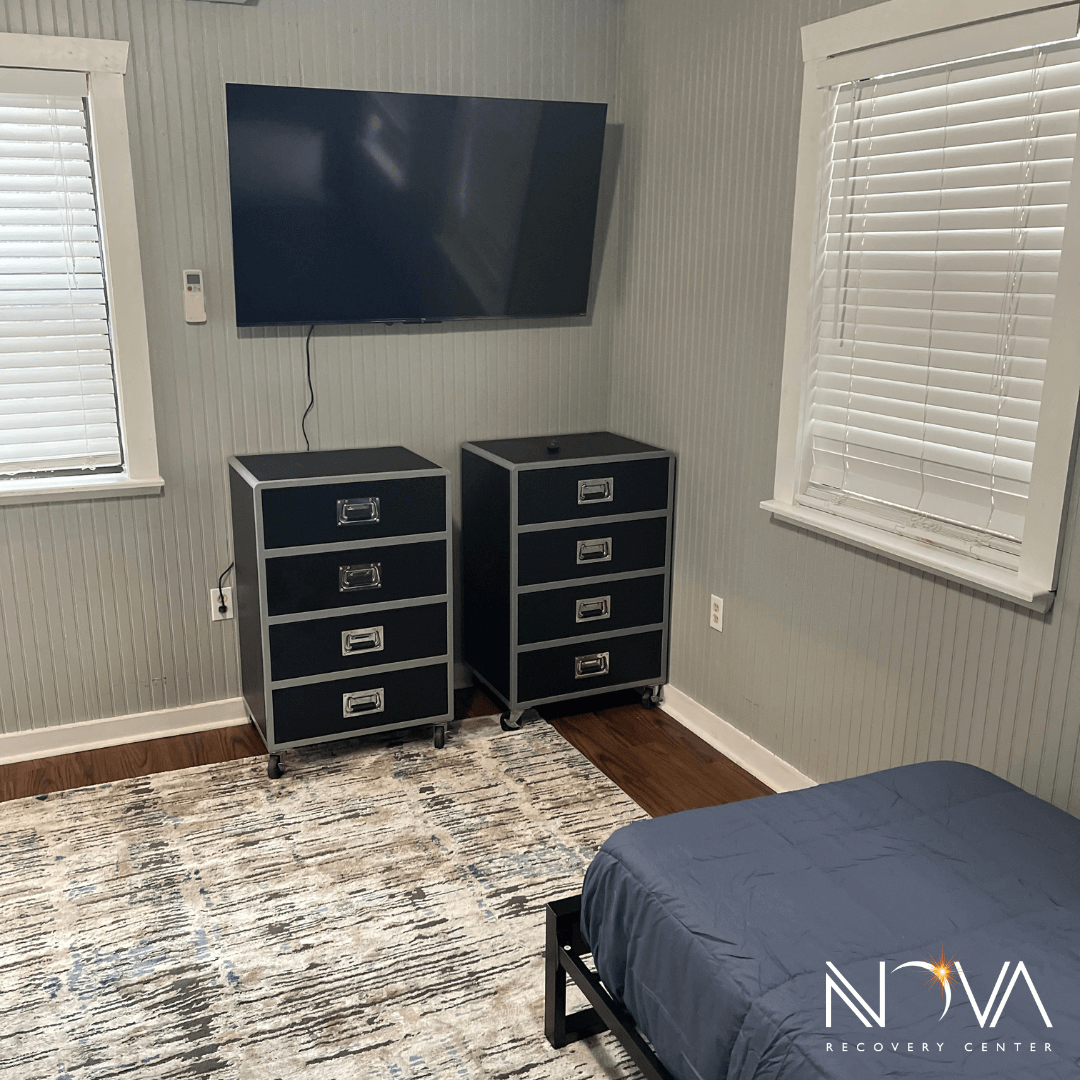
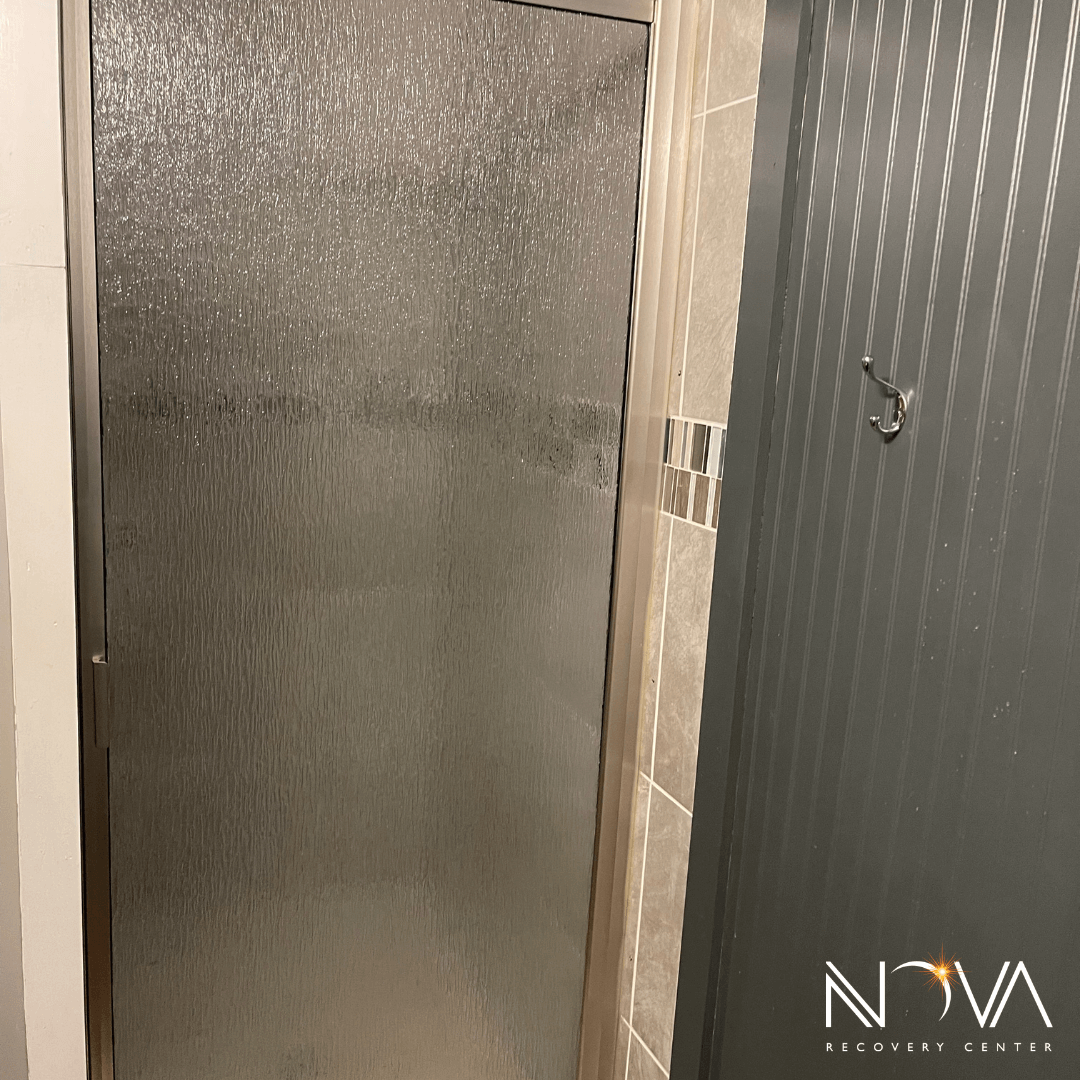
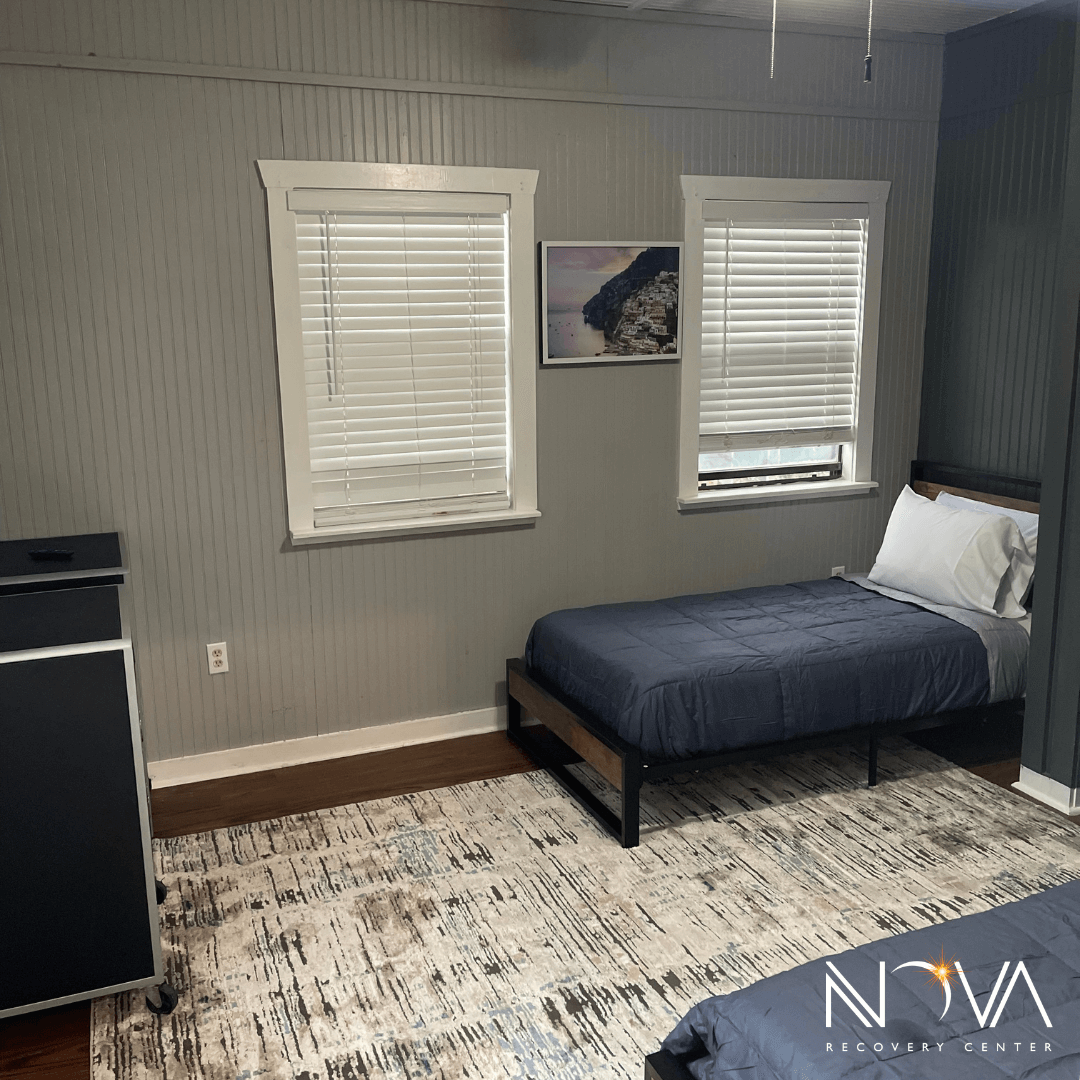
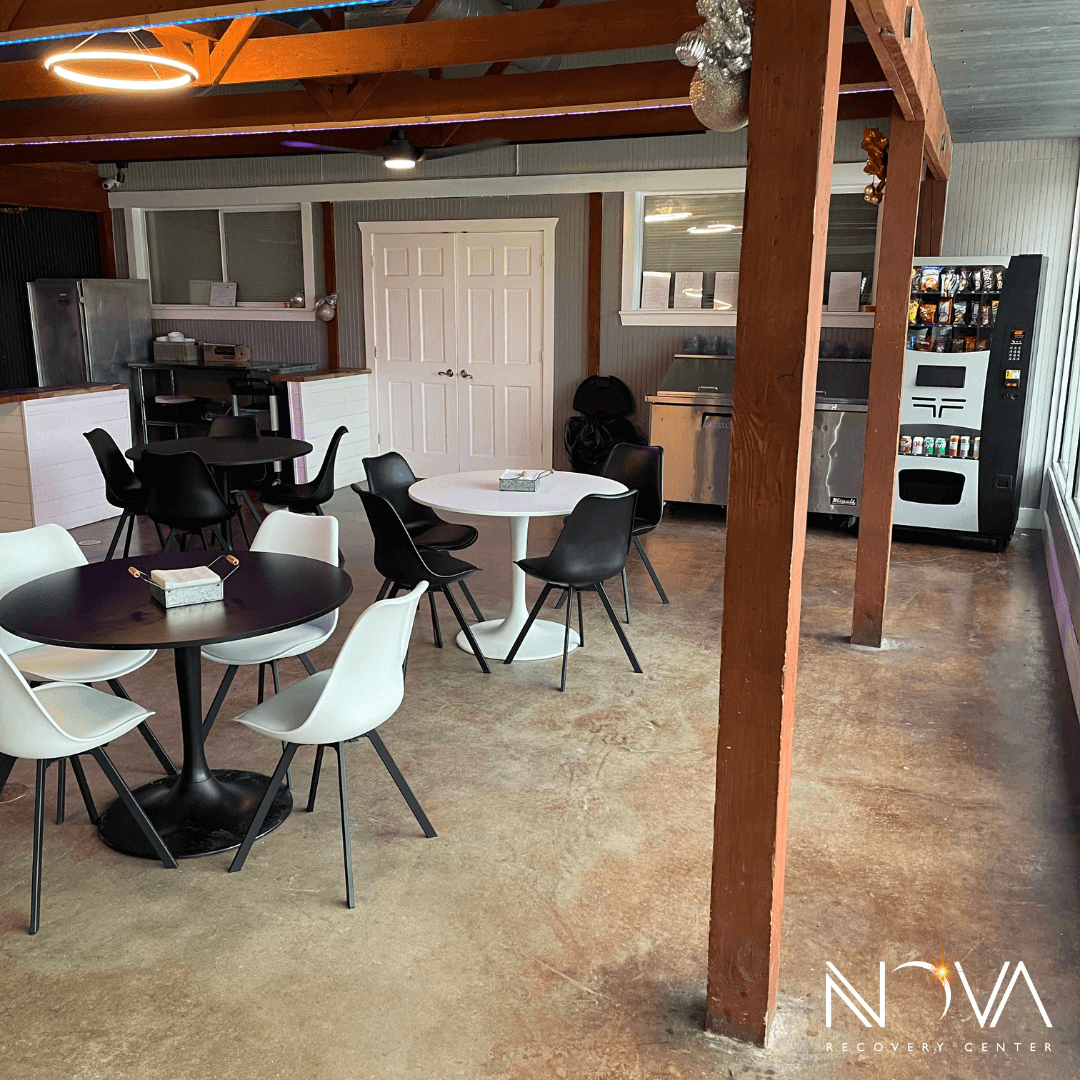
A structured setting can help stabilize sleep, stress, and routine while clinicians review symptoms and medications. Nova’s Austin residential inpatient rehab program provides 24/7 support and a consistent schedule, which can be helpful when symptoms are complex.
To understand costs and coverage, you can verify your insurance coverage and admissions options before starting treatment.
If you prefer residential care in a quieter setting near the Hill Country, Wimberley inpatient rehab offers structured support with a focus on long-term recovery.
If you want to talk through symptoms and next steps, you can contact our team to discuss treatment and next steps.